
| Home Page | Overview | Site Map | Index | Appendix | Illustration | About | Contact | Update | FAQ |
 |
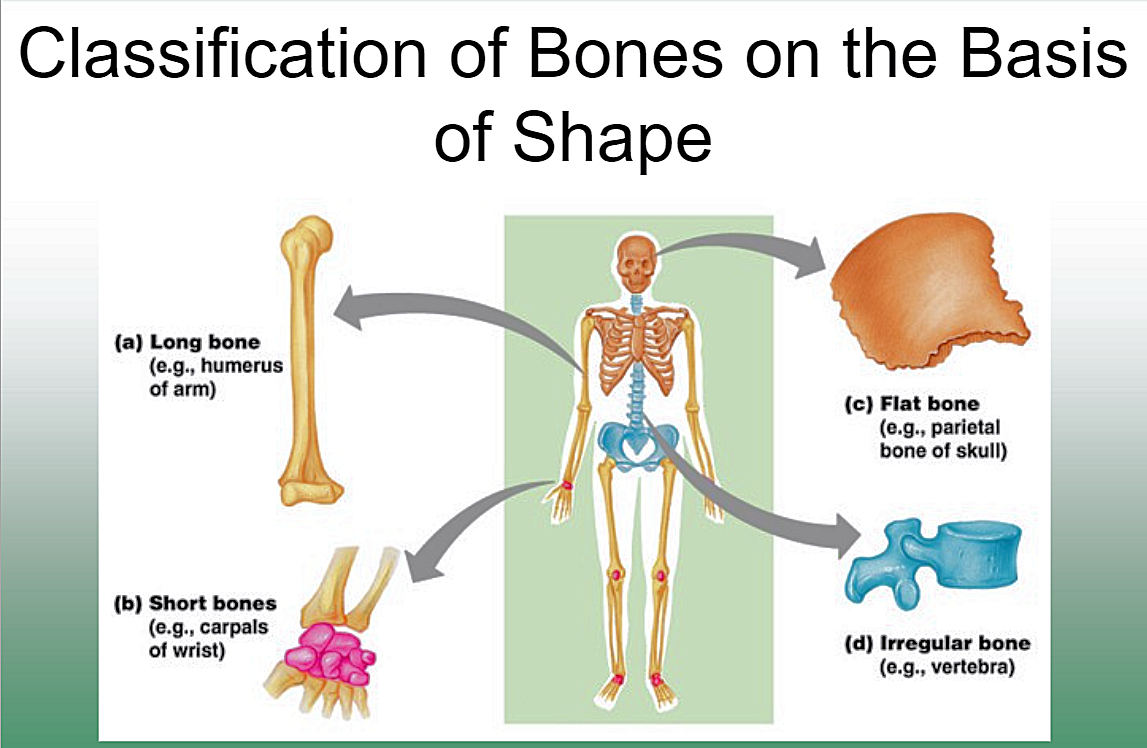
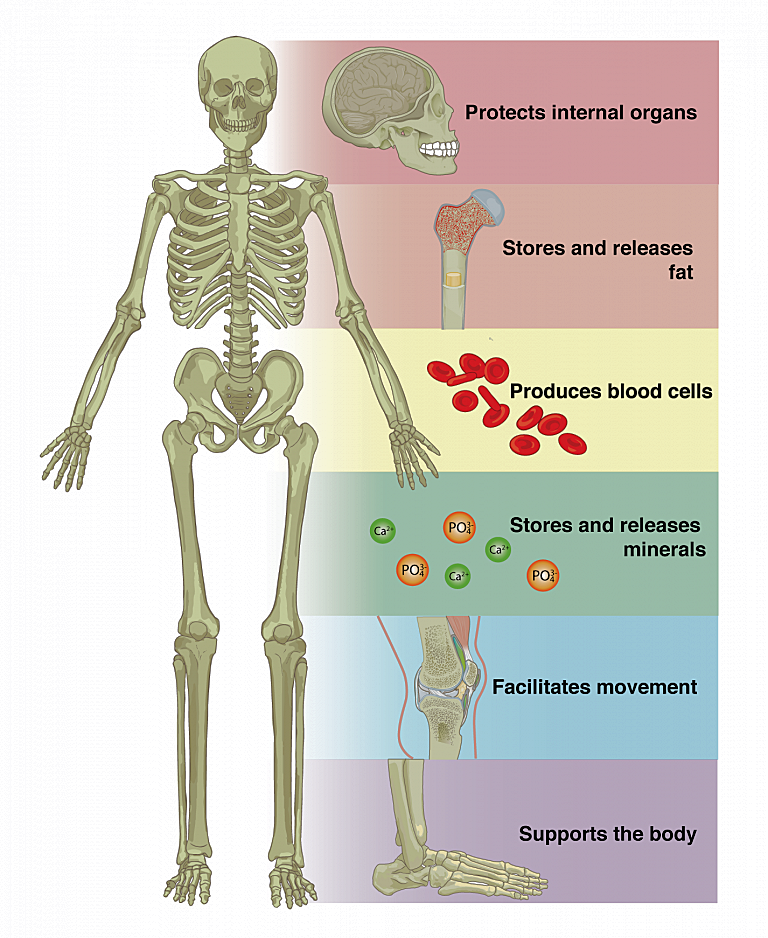
Bones can persist for a long time, potentially thousands of years, under favorable conditions like dry environments or in certain types of soil. Generally, there are 4 different types (see Figure 10-13h1); the long bone is the strongest. Bones serve many vital function (see Figure 10-13h2); here's a list provided by ChatGPT (in italic) : |
Bone Fossil |
 |
 |
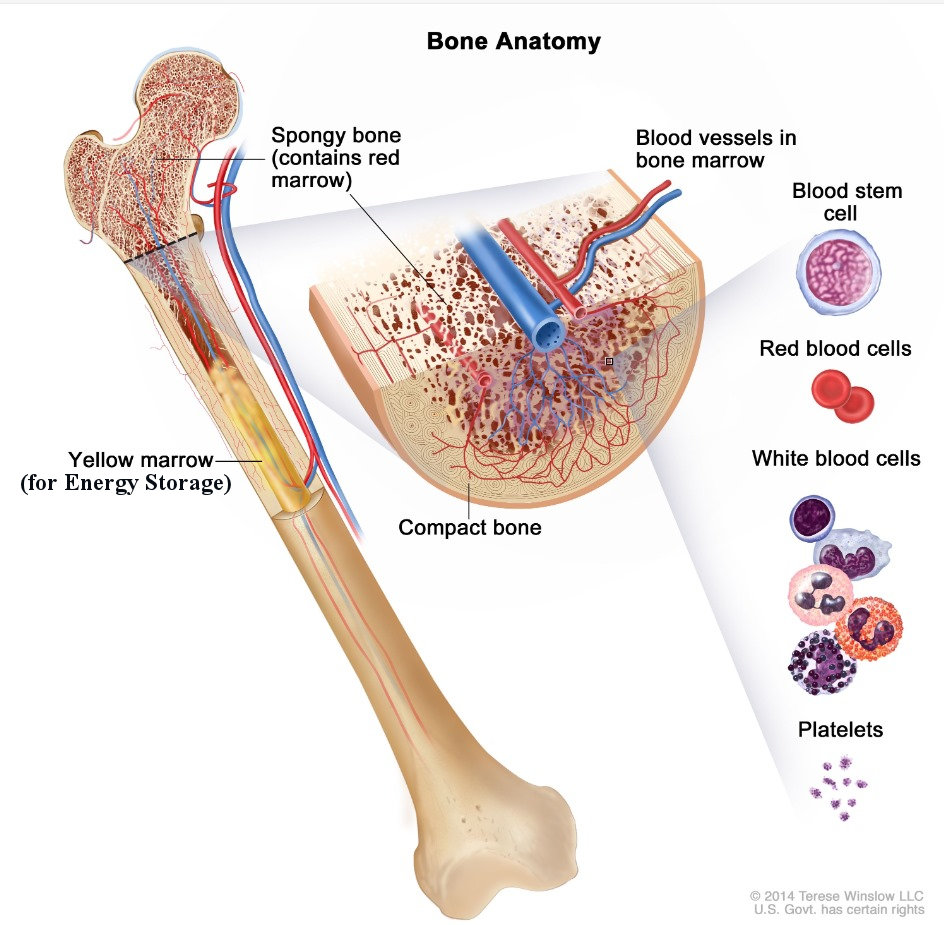
6. Blood Cell Production: Within the bone marrow, specialized cells called hematopoietic stem cells produce various types of blood cells, including red blood cells, white blood cells, and platelets. This process is known as hematopoiesis and occurs primarily in the marrow of certain bones, such as the pelvis, sternum, and long bones. The red marrow found within these bones contains hematopoietic stem cells that continuously produce red blood cells, white blood cells, and platelets throughout adulthood. |
Figure 10-13h1 Types of Bone |
Figure 10-13h2 Uses |
 |
This transition may have provided several advantages, such as increased flexibility, greater mobility, and improved protection of internal organs. The shift from exoskeleton to endoskeleton likely occurred gradually over evolutionary time, driven by environmental pressures and the need to adapt to changing habitats and ecological niches. |
Figure 10-13h3 Skeleton |
 |
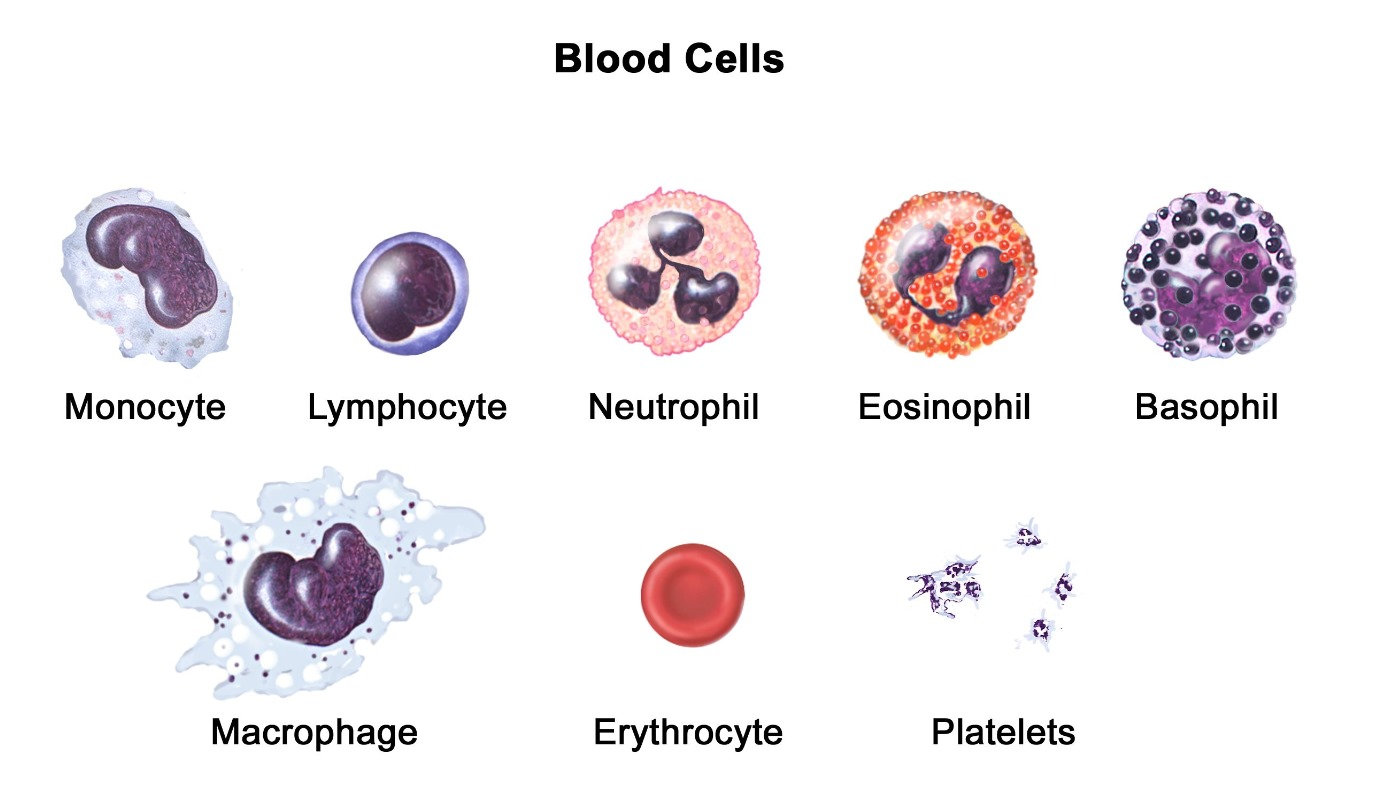 |
3. Platelets (Thrombocytes): * Function: Essential for blood clotting (hemostasis) to stop bleeding when blood vessels are damaged. * Structure: Platelets are small, irregularly shaped cell fragments derived from the fragmentation of megakaryocytes in the bone marrow. * Role in Hemostasis: Platelets adhere to the site of vascular injury, aggregate to form a plug, and release factors that promote blood clot formation. |
Figure 10-13h4 Bone Marrow |
Figure 10-13h5 Blood Cells [view large image] |
These blood cells work together in a coordinated manner to maintain the body's health and protect against pathogens and injuries. It becomes fatal if blood loss is over 40%.
See "Powerful imaging shows blood cells made in bone" and Figure 10-13h6 |
 |
The March, 2024 article "Resilient anatomy and local plasticity of naive and stress haematopoiesis" on haematopoiesis response to "insult" (such haemorrhage, bacterial infection and during ageing) is followed by the April, 2024 article "Depleting myeloid-biased haematopoietic stem cells rejuvenates aged immunity", which demonstrates that increasing certain type of Haematopoietic Stem Cell (HSC) would enable aged mice to restore characteristic features of a more youthful immune system. It seems that "haematopoietic" is an active research subject because it is directly related to aging (see Figure 10-13h7). |
Figure 10-13h6 Production |
 |
The production sites of hematopoiesis, where blood cells are formed, changes throughout a person's lifetime due to developmental and physiological factors. The progression involves the commplicated interaction between 2 types of stem cells, see "Hematopoiesis during Ontogenesis, Adult Life, and Aging". Figure 10-13h7 shows the changes during the lifetime in term of cellularity (number of cells in a given tissue sample in term of precentage), while ChartGPT provides a short description (in italic) : |
Figure 10-13h7 Progression |
 |
The preference for bone marrow over the spleen in mammals may be due to factors such as the bone marrow's larger capacity for hematopoiesis and its more specialized microenvironment, which supports the proliferation and differentiation of hematopoietic stem cells. Additionally, the bone marrow provides a more protected environment for blood cell formation compared to the spleen, which is more susceptible to damage and infection. Actually, the lymph node in human can be considered as the miniature version of the spleen (see Figure 10-13-h6). |
Figure 10-13h8 Spleen |
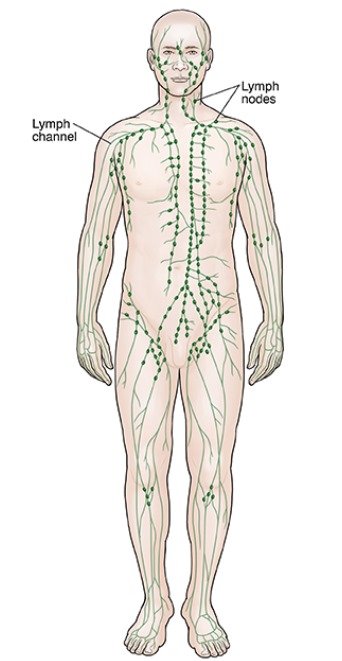 |
1. Filtration: Lymph nodes act as filters, trapping and removing foreign particles, such as bacteria, viruses, and cellular debris, from the lymph fluid before it returns to the bloodstream. This helps to prevent the spread of infections and diseases throughout the body. 2. Immune response: Lymph nodes are hubs for immune cell activation and coordination. They contain various types of immune cells, including lymphocytes (B cells and T cells), macrophages, and dendritic cells. When foreign substances are detected in the lymph fluid, immune cells within the lymph nodes become activated, initiating an immune response to eliminate the threat. 3. Production of lymphocytes: Lymph nodes support the production and maturation of lymphocytes, which are crucial for the adaptive immune response. B cells mature and differentiate into plasma cells (which make antibodies to fight bacteria and viruses, to stop infection and disease). |
Figure 10-13h9 Nodes |
 |
3. Pressure Changes from Breathing: The act of breathing creates pressure changes in the thoracic cavity (chest). These changes help move lymph fluid, especially through the larger lymphatic ducts (like the thoracic duct), as the pressure gradients assist in drawing the lymph upward toward the subclavian veins, where it reenters the bloodstream. 4. Body Position: Gravity can affect lymph flow, particularly in the lower extremities. |
Figure 10-13h10 Lymphatic System [view large image] |
See "Lymphatic System- Organs, Functions, Diseases". |
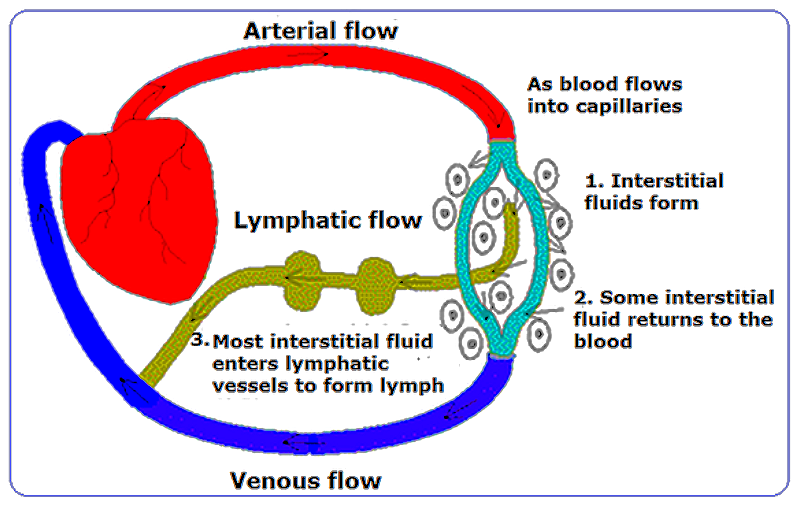 |
In general, the lymphatic system efficiently cleans up and filters waste within a few days under normal conditions. Physical activity, breathing, and overall health can speed up this process. |
Circulation |
+ Flow of Lymph Video |
 |
2. Lymphatic System Function: The lymphatic system primarily helps in removing waste products, toxins, and unwanted materials like bacteria or viruses from the body. It doesn't target healthy, non-pathogenic cells like melanocytes unless there is an abnormal change, such as malignancy. 3. Mole Location: Moles are typically located in the dermis and epidermis layers of the skin, where they integrate with normal skin tissue. The lymphatic system is more involved in the removal of fluids, immune cells, and waste products from deeper tissues rather than surface-level changes like moles. 4. Stable Nature of Most Moles: Most moles are benign, stable structures. Since they don't pose a threat or signal damage, the body has no mechanism to remove them naturally. |
Figure 10-13h11 Moles [view large image] |
In cases where moles need to be removed, such as for cosmetic reasons or if they show signs of becoming cancerous (e.g., melanoma), they are typically excised surgically. See more about "Moles". |